- Your Alliance for all your CHC needs.
- (386) 673-9846
- info@thechcalliance.com
Maternal Health in America: A Call to Action in the Face of Alarming Statistics

12 Days of a CHC Christmas
December 14, 2023
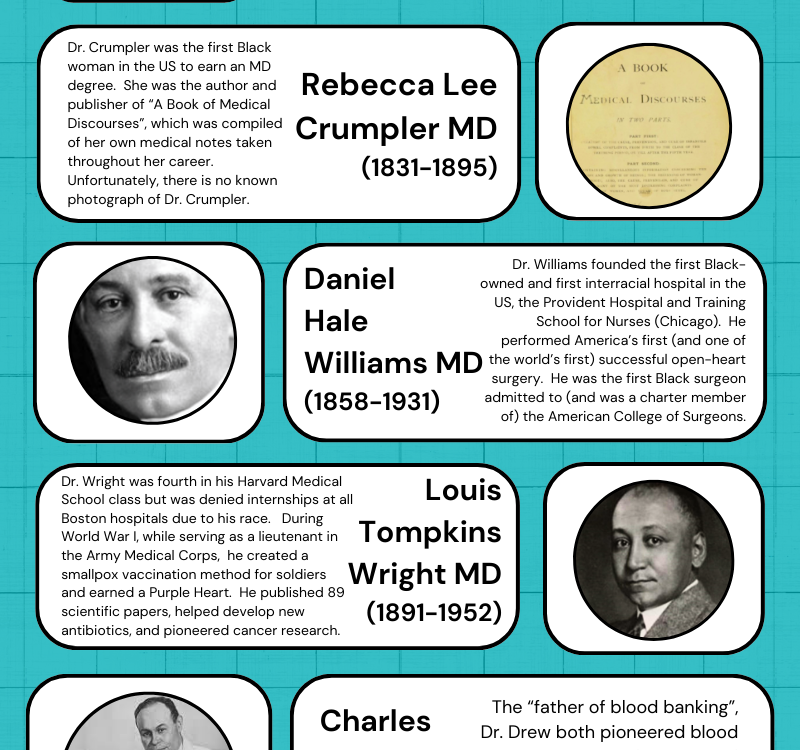
8 American Medical Pioneers
February 16, 2024Maternal Health in America: A Call to Action in the Face of Alarming Statistics
In September, HRSA (Health Resources and Services Administration) announced that they were investing nearly $90 million to support the White House Blueprint for Addressing the Maternal Health Crisis (which was introduced in June 2022).
While we’re excited for the mothers and infants who will receive treatment because of these funds, we recognize that America’s maternal health crisis deserves as much attention as possible. With that in mind, we wanted to share some facts about the current state of maternal health in the United States. And, in keeping with our FQHC focus, we’re also including links to two HRSA funding opportunities that are part of their investment.
The World Health Organization (WHO) defines maternal death as “the annual number of female deaths from any cause related to or aggravated by pregnancy or its management (excluding accidental or incidental causes) during pregnancy and childbirth or withing 42 days of termination of pregnancy, irrespective of the duration and site of the pregnancy.”
According to the OECD (Organisation for Economic Co-operation and Development), which compiles and reports cross-nationally for 38 high-income countries, the United States has the highest per-person health care spending but the lowest life expectancy at birth and the highest maternal and infant mortality rates of the OECD nations.
The OECD average for maternal mortality is 9.8 deaths per 100,000 live births. Our rate is 23.8—nearly double that of New Zealand, which has the next highest rate (13.6). In fact, the U.S. maternal mortality rate is nearly 12 times that of Australia (2.0), 4 times that of the United Kingdom (6.5), and 3 times that of our neighbor to the north, Canada (8.4). And let’s not even compare ourselves to Norway (1.6).
In the United States, the Centers for Disease Control and Prevention (CDC) suggests the rate is even higher. According to the CDC, the maternal mortality rate rose from 20.1 deaths (per 100,000 live births) in 2019 to 32.9 deaths in 2021.
It’s easy to understand that we have a health crisis on our hands. In an interview with USA Today, Dr. Elizabeth Cherot, March of Dimes Senior Vice President and Chief Medical and Health Officer, had this to say: “We’re going in the wrong direction. We remain the most dangerous developed country to give birth in, and when you look at this particular data, it’s getting worse—and it’s getting worse for black and brown women.”
The maternal mortality rates in the U.S. for mothers of color are staggering. For black and AIAN (American Indian/Alaskan Native) mothers, the mortality rates were three times higher when compared to white women.
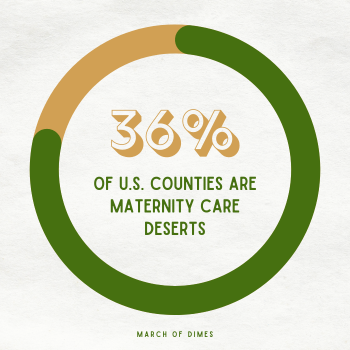 Even more sobering is the idea of maternity care deserts in the U.S. In their 2022 report, “Nowhere to Go: Maternity Care Deserts Across the U.S.”, the March of Dimes reports that 4.7 million women in the U.S. live in counties that have limited maternity care access. They found that 36% of all U.S. counties can be designated as maternity care deserts, with limited or no health care services for women during pregnancy, delivery, and postpartum.
Even more sobering is the idea of maternity care deserts in the U.S. In their 2022 report, “Nowhere to Go: Maternity Care Deserts Across the U.S.”, the March of Dimes reports that 4.7 million women in the U.S. live in counties that have limited maternity care access. They found that 36% of all U.S. counties can be designated as maternity care deserts, with limited or no health care services for women during pregnancy, delivery, and postpartum.
FQHCs were created to meet the healthcare needs of underserved and diverse populations in the U.S. They’re on the frontlines of this fight to lower the maternal mortality rate. “About two-thirds of FQHC clinic networks include a site that provides prenatal care directly, and the rest refer patients to other clinics. Racial disparities in access to care and birth outcomes are diminished among patients served by FQHCs relative to the general population.”
Sometimes it can be so easy to focus on the problem directly in front of you that you miss the big picture. We know that each healthcare professional connected with an FQHC or CHC that provides prenatal care could share stories of mothers (and infants) who were saved from becoming statistics because their condition was caught in time. We also know that, because of you, the patient populations you serve don’t have to struggle in a maternity care desert.
We celebrate you, and we urge you to continue the fight to lower the U.S. maternal mortality rate. If you’re an FQHC that doesn’t currently offer prenatal care, that could be a goal—especially if you live in or near a county that’s considered a maternity care desert. Perhaps you could start by finding out how your organization can offer support to midwives and doulas in your area.
 As promised, here are links to two HRSA grant programs that are part of their $90 million investment to address the maternal health crisis in the U.S. According to HRSA’s site, both grants are open to organizations that are in the United States, public or private, community-based, and/or tribal (governments, organizations). Be sure to share this information!
As promised, here are links to two HRSA grant programs that are part of their $90 million investment to address the maternal health crisis in the U.S. According to HRSA’s site, both grants are open to organizations that are in the United States, public or private, community-based, and/or tribal (governments, organizations). Be sure to share this information!
Healthy Start Initiative: Eliminating Disparities in Perinatal Health
Deadline to apply: 12/15/23.
Supporting Healthy Start Performance Project
Deadline to apply: 12/29/23.